The knowledge to treat you better
The best doctors never leave medical school.
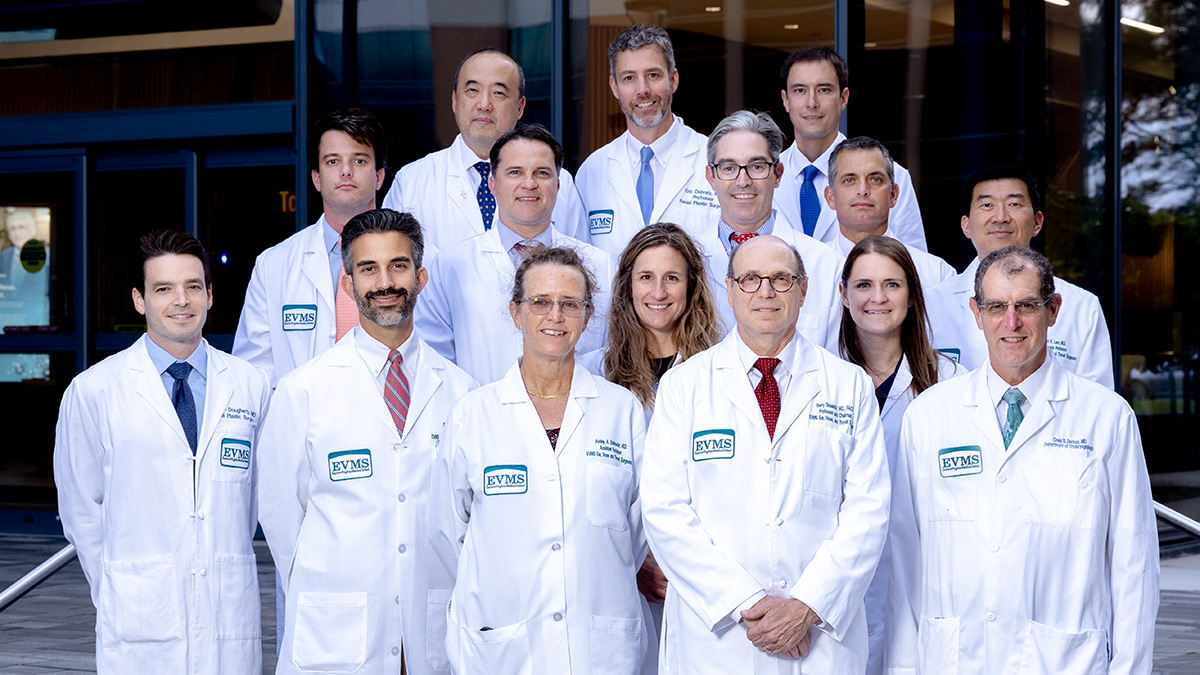
EVMS Ear, Nose and Throat Surgeons are here to provide superior and compassionate care for patients of all ages. As part of an academic medical center, we are able to offer the most advanced treatments for disorders of the ear, nose, head and neck. Our physicians are highly skilled, fellowship-trained experts in their chosen subspecialties.
Our offices are conveniently located throughout Hampton Roads including Norfolk, Virginia Beach, Chesapeake and Newport News. We strive to help you feel comfortable and confident as a patient. After all, we are the doctors who teach the doctors.
The EVMS Difference
As an academic medical center, EVMS offers the most advanced treatment options, comprehensive services, award-winning medical research and specialized patient-care programs. We continuously collaborate with national and international partners to develop medical technologies for the future. Choose providers with the knowledge to treat you better at EVMS Medical Group.
Featured providers
Frequently asked questions
This depends on what kind of insurance you have.
If you have an HMO, you must:
- Get a referral from your primary care physician before calling to make an appointment.
- Make sure your referral has not expired. Many are good for only 30 days, so be sure to check before you come to your appointment.
- If your referral has expired, call your primary care physician and explain your situation. In most cases, your doctor will provide a new or extended referral.
- Bring the referral with you to the appointment. If you do not have a referral, or if the referral you have is expired, your HMO will not pay for your appointment.
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
You may reach your doctor's office Monday - Friday between 8 a.m. and 5 p.m. at the regular office number.
River Pavilion Office - 757-388-6200
Princess Anne Office - 757-689-8500
CHKD Offices - 757-668-9327
After regular office hours and on weekends call 757-388-6200 to reach the answering service and the doctor on call.
Each department has various required paperwork for patients. Ask your provider's office or visit the department's page to download the proper forms.
Please print and complete the forms and bring them to your first appointment with you.