Women's Healthcare
EVMS OB/GYN believes all women have the right to expert, safe, compassionate and equitable women’s healthcare. Our mission is to provide accessible, evidence-based, patient-centered care enhanced by collaboration, research, advocacy, community partnerships and education.
You deserve providers who understand your unique healthcare needs. Our fellowship-trained obstetrician-gynecologists, maternal-fetal specialists, urogynecologists, and gynecological surgeons provide high-quality care for women of all ages.
Whether you're an adolescent, post-menopausal or somewhere in between, your health needs come first. Our women's healthcare team is committed to making sure we support you through every stage of your life. We are honored to be your chosen provider for exceptional, patient-centered care.
- General Obstetrics and Gynecology EVMS OB/GYN division offers you the individualized gynecological care that you deserve. From contraceptive counseling to menopause management, our providers can diagnose, treat and manage your most personal health issues.
- Obstetrical / Pregnancy Care Our OB/GYNs offer you the maternity care you deserve, providing compassionate care and support before, during and after your pregnancy. We provide preconception counseling, prenatal care and postpartum services.
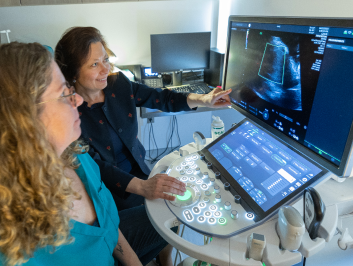
- Maternal-Fetal When risk factors threaten to complicate your pregnancy, you can place your trust in our EVMS’s Maternal-Fetal Medicine (MFM) division. Our MFM team is uniquely positioned to provide full-scope, high-quality care to the pregnant patients of Hampton Roads.
- Urogynecology Our goal in the Urogynecology (URO) division at EVMS is to restore lost function to our patients, whether pathological, physiological, menopause or prolapse-related. Our URO treatment options range from physical exercises to medications to reconstructive surgery.
- Gynecologic Surgery If your condition needs surgical care, our Minimally Invasive Gynecological Surgery (MIGS) division at EVMS is here to provide innovative, quality care. We offer a range of treatment and surgery for complex gynecologic conditions.