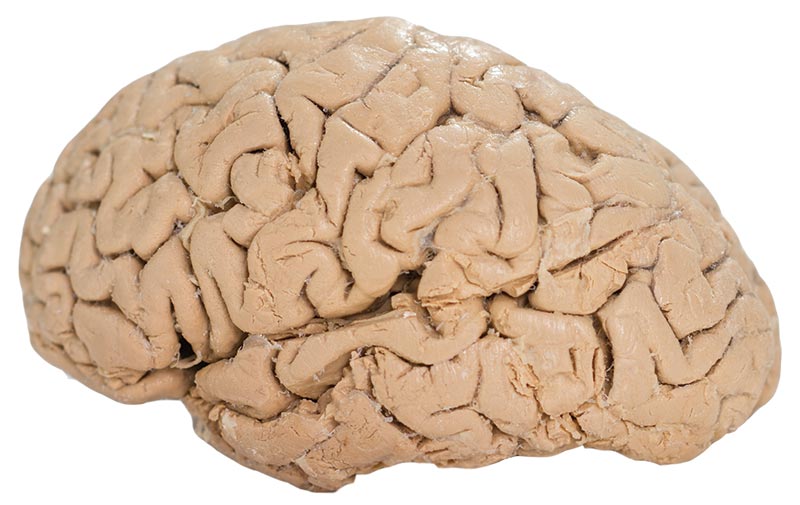
The delicate skeletal structure of a fetus at 12 weeks rests on a table in the lab. Its tiny ribs — smaller than the tip of a fingernail — curve toward chest and back bones. Beside the model sits an adult inner-ear, or temporal, bone, twice the size of the fetus, yet still intricate in detail.
Here, in this lab, science is technology is art. And at its very center sits Miro Kirov.
"This is artistry," he says. "We make beautiful things."
Always interested in the human form, Mr. Kirov, MPS, is a sculptor. But today he isn't using clay. He demonstrates his talents in a much different medium: 3D printing.
"I must find every intricate detail, every curve and turn, and then teach the printer how to create it," he explains.
He talks without looking up from his computer screen, where he is bringing a virtual model of a temporal bone to life. As he clicks here, then there, the shape zooms in and out. The low hum of a printer fills the silence between his sentences.
"This is the fusion of art and science," Mr. Kirov says, "with the added complexity of the human form."
It's revolutionary, yet it is not new technology.
In fact, 3D printing has been around since 1987 and was first used by car and airplane manufacturers to design complicated parts and then print out prototypes. Today, inexpensive 3D printers are commonplace and can be used at home to make screws, ear buds and even toys.
Stories of how 3D printing is changing the landscape of medicine are now also commonplace. At many hospitals, surgeons use 3D renderings of a patient's unique anatomy to practice procedures before they enter the operating room. And 3D printers are being used to custom fit parts, such as prosthetics and knee implants.
Yet there is still much to discover in this marriage of technology and medicine.
"The way we see, understand and then interpret human anatomy for teaching and inevitably for patient care has changed," says Craig Goodmurphy, PhD, Professor of Pathology and Anatomy and Director of the EVMS 3D printing lab.
X-rays, CT scans and handheld ultrasound were all game changers. So, too, he says, is 3D printing.
"This is complex medical engineering, and the possibilities are endless."
Dr. Goodmurphy employs various 3D projects in his lab that allow students and residents to perfect their techniques. For example, he is developing model temporal bones — a cost-effective option that would enable residents more frequent practice with drilling techniques. Additionally, life-sized eye models can be filled with gels and liquids to simulate human tissue for suturing practice.
Much of his focus is combining 3D-printed items with other materials to enhance ultrasound practice. Several of his research projects are being field-tested at medical schools across the country, including the University of Virginia School of Medicine and Vanderbilt School of Medicine.
"And all this is being done with a less expensive 3D printer," Dr. Goodmurphy says. "Imagine what could be accomplished with more funding.
Practice makes perfect
The human body has always been the best teacher. Technology, however, is expanding the ways we can teach future health and medical professionals about it.
Human anatomy hasn't changed," says Carrie Elzie, PhD, Assistant Professor of Pathology and Human Anatomy. "The way we look at it has."
Dr. Elzie, Director of the Contemporary Human Anatomy Program, a new master's program that enrolls its first class this summer, says 3D printing, alongside skills such as plastination (See Plastination sidebar on next page) and virtual dissection, will certainly have its place in the new curriculum.
And Dr. Goodmurphy is working to include elements of 3D printing in his anatomy courses.

"We have the opportunity to create models that are specific to complicated pathology, and we can do it in a more cost-effective way," he says. "While the use of cadavers is still very important, 3D printing can enhance those lessons and allow for multiple exposures and repetitive practice."
Take, for example, a 3D-printed fetus suspended in a gel block. This enables students to conduct repeated vaginal ultrasounds to determine the size and age of a fetus without a patient enduring an exam over and over again. Plus, the model fetuses can depict an array of conditions detectable by ultrasound.
"This doesn't replace live practice," Dr. Goodmurphy says. "It supports it."
Students and residents also are developing research projects using 3D printing. Chelsea Allen, MD Class of 2018, spent last summer working in the lab with Dr. Goodmurphy and Shannon McCole, MD (Ophthalmology Residency '97), Chair of Ophthalmology. The project: to 3D-print molds for models that simulate problems in the eye, which can be found via ultrasound.
These models are inexpensive and eliminate the biohazard issues of using real human or porcine eyes, Dr. McCole says. More important, they give students an opportunity for frequent hands-on practice early in their medical-school careers.
Ms. Allen agrees.
"EVMS has been on the forefront of ultrasound education," she says, "and I think adding 3D printing as another pillar of our education shows how innovative this school is. The technology is advancing and so is EVMS."
Printing personalized parts
Modern medicine keeps developing technology to rebuild the human body. Earlier this year, a study published in the journal Nature Biotechnology outlined the success of bioengineers who used 3D printing to craft an ear from what they called an "integrated tissue and organ printing system." The ear was then implanted under the skin of a mouse. Not only did the 3D-printed ear live for several months, it also grew cartilage tissue and blood vessels.
Another study, this one published in the Proceedings of the National Academy of Sciences, details how engineers have 3D-printed tissue that mimics the structure and function of the liver.

"To me, 3D printing was a black box," Barry Strasnick, MD, says, "something that was science fiction. You could make a Match Box car or a cell-phone case, but now we are talking about being able to print actual human replacement parts. That is evolution; it's not a gimmick anymore."
Dr. Strasnick, Professor and Chair of Otolaryngology-Head and Neck Surgery, now embraces the technology and is seeking grants and funding to expand 3D printing at EVMS.
He is collaborating with Dr. Goodmurphy on developing 3D temporal bones so that residents have an endless and more cost-effective supply. On the patient side, he is interested in expanding his 3D projects into bite guards, custom tracheotomy tubes, artificial hearing bones and CPAP masks. He also wants to explore using 3D-printed tracheas lined with stem cells to spur tissue growth.
"Imagine that we have to remove your mandible," Dr. Strasnick says, "and instead of waiting weeks for a replacement to be perfected to fit, we could print your replacement right there and install it. It's like saying this is your jaw we are taking out and here is an exact copy that we are putting in."
At the Hampton VA Medical Center, Jose Morey, MD, Assistant Professor of Internal Medicine at EVMS, is confident 3D printing could have an immediate impact on the Hampton Roads military community. Dr. Morey and Dr. Goodmurphy are exploring grants and funding that would create a joint manufacturing lab stocked with high-quality 3D printers. This lab would provide veterans with custom-fitted prosthetics.
"Right now, amputees have to wait several months and spend hundreds of thousands of dollars to get their prosthetics," Dr. Morey says. "By using 3D printers, we could reduce the wait time from months down to days and the costs down to just hundreds."
A joint lab would also save agencies like the Veterans Administration millions of dollars.
"We are ready to put the boots on the ground and get to work because we know we can have real-world, immediate impact," he says.
However, the high cost associated with advanced 3D printers and the lack of structured regulatory frameworks and reimbursement policies are, for the time being, blocking widespread adoption of 3D-printing labs in hospitals.
Still, surgeons like Dr. Strasnick argue that using 3D technology would reduce the duration of surgery and anesthesia exposure, assist in better pre-surgery planning and improve overall practice. Plus, 3D printing on a larger scale could be the answer to remove the one-size-fits-all treatment parameters.
"We could ensure that patients get custom-fit items, not just what the standard size is that we keep on the shelves," Dr. Strasnick says. He uses tracheotomy tubes as an example; each tube can cost upward of $90 and comes in limited sizes.
"If we could print your tubes before you leave the hospital," he says, "then we don't have to store all those sizes, and it costs significantly less. We could save the patient money, the hospital money and us money. In the long run, it's a real win-win-win."
For Mr. Kirov, the economics and policies related to 3D printing are matters for others to tackle. Here, in this lab, he is an artist, sculpting beautifully delicate models from complex technology.
This is his science, his medium, his art.